NICE issues positive guidance for minimally invasive weight loss procedure
22 February 2024
People living with obesity in the UK can be offered endoscopic sleeve gastroplasty (ESG), a minimally invasive treatment for weight loss, according to updated guidance issued by the National Institute for Health and Care Excellence (NICE). This is the first time the treatment will be available on the National Health Service (NHS), which recorded over 1 million hospital admissions linked to obesity in England in 2022/23 an increase of eight per cent on the previous year.1
The guidance is a significant step forward in obesity care because they provide patients with another option for reaching a healthy weight outside of prescription weight loss drugs or bariatric surgery. NICE said that ESG is safe in the short and long term when combined with lifestyle changes and could help with weight loss in people, who have not lost weight with lifestyle modifications alone, and who are not suitable or do not wish to undergo bariatric surgery 2.
Expanding treatment options
NICE reviewed the evidence on the safety and efficacy of ESG, which included the Apollo OverStitch™ Endoscopic Suturing System3 from Boston Scientific. Patients selected by a multidisciplinary team can be offered this procedure in specialist centres by a clinician, who has received specific training. Under the NHS’s long term plan, tackling obesity is a priority as it is estimated that 26% of adults in England are living with obesity and a further 38% are overweight.3 Other health conditions are linked, such as cardiovascular disease and type 2 diabetes.4 Patients also report that obesity affects their mental health and emotional well-being. The NHS spends an estimated £6.5 billion a year on obesity which is the second biggest preventable cause of cancer.5
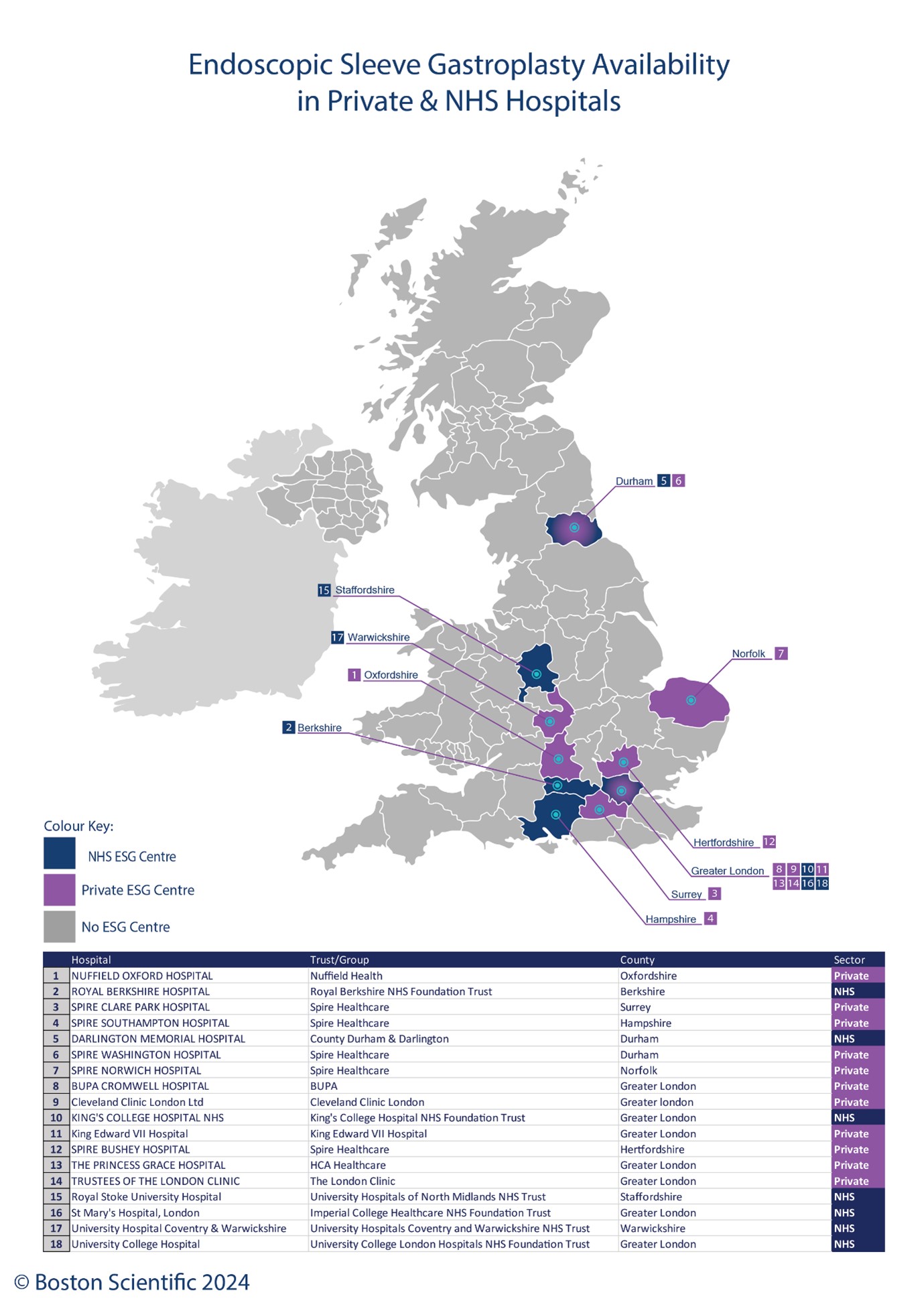
Currently ESG is available in seven NHS hospitals including London, Berkshire, the Midlands, and County Durham [see Figure 1].
The procedure, conducted under general anaesthetic, takes around 90 minutes to complete and involves a flexible endoscope with a suturing device being passed through the patient’s mouth into the stomach.
Transforming patient outcomes
Initially carrying a body weight of 98 kg , Joanna, a tattoo artist, has had an ESG procedure to lose 24 kg. She tried lots of lifestyle changes which helped with some weight loss but inevitably gained the weight back which was affecting her confidence, health, and emotional well-being. “I started to struggle with my weight when I became a tattoo artist because my weight went from living a fairly active life to from where I was up and down a lot to sitting down all day every day,” said Joanna. “Since having the procedure I don’t feel like I don’t really have to try to keep the weight off anymore. It’s just very natural and very instinctive.”
 “The NICE guidance is fantastic news for patients by giving them another treatment option,” said Dr Jamie Kelly, Upper Gastro-Intestinal lead surgeon at University Hospital Southampton. “Increasing patient access to treatment requires making them aware of this option and training more surgeons and physicians to perform the procedure.”
“The NICE guidance is fantastic news for patients by giving them another treatment option,” said Dr Jamie Kelly, Upper Gastro-Intestinal lead surgeon at University Hospital Southampton. “Increasing patient access to treatment requires making them aware of this option and training more surgeons and physicians to perform the procedure.”
“Endoscopic sleeve gastroplasty appeals to people as, according to NICE, it is a safe, non-invasive procedure which allows them to return to normal life sooner than bariatric surgery,” said Ken Clare, director of bariatric and metabolic surgery services at Obesity UK, a charity which supports 20,000 members living with this disease. “ESG may improve access for people in areas where treatment options are limited by the postcode lottery of services for weight management.”
Data insights
Clinical studies show that 77% of patients lost a quarter or more of their original weight a year after having the ESG procedure.7 “Women in the UK experience higher obesity rates than men. Data also shows this is the case in some ethnic minority groups8, both of which lead to health inequalities as obesity is a serious chronic disease,” said Astrid Monteau, vice president EMEA of endoscopy at Boston Scientific. “The publication of NICE’s guidance offers a pathway to reduce pressure on the healthcare system as patients have shorter recovery times and because this procedure can be performed as a day case.”
References
1Part 1: Hospital admissions - NHS Digital
2Endoscopic sleeve gastroplasty - NICE